AARP Eye Center

LITTLE ROCK— AARP_FS_LTSS2017_Arkansas_061017, and AARP warns much more must be done, at an accelerated pace, to meet changing demographic demands. Specific areas of concern in Arkansas include effective transitions between nursing homes, hospitals and homes.
These findings are according to a new, comprehensive state-by-state Scorecard from AARP with support of the nation’s leading organizations behind quality long-term care, The Commonwealth Fund and SCAN Foundation.
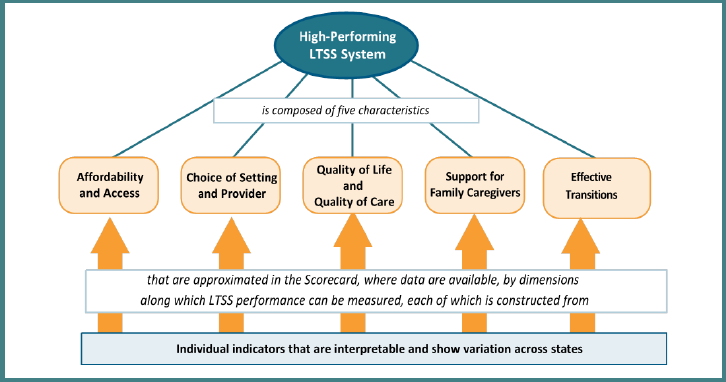
Picking Up the Pace of Change: A State Scorecard on Long-Term Services and Supports for Older Adults, People with Physical Disabilities, and Family Caregivers, 2017 Edition —the third in a series of reports—ranks each state overall and on 25 specific indicators in 5 key dimensions: affordability and access; choice of setting and provider; quality of life and quality of care; support for family caregivers; and effective transitions between nursing homes, hospitals and homes.
“The vast majority of older Arkansans want to live independently, at home, as they age—most with the help of unpaid family caregivers,” said Ness Nehus, Associate State Director of Advocacy of AARP Arkansas, which serves more than 310,000 members age 50 and older in Arkansas. “Even facing tight budgets, Arkansas is making some progress to help our older residents achieve that goal. However, this Scorecard shows we have more to do, and we need to pick up the pace.”
A fact sheet showing how Arkansas fared in each key dimension and specific indicator may be is available AARP_FS_LTSS2017_Arkansas_061017. The full state Scorecard, along with an interactive map of state rankings and information, is available at www.longtermscorecard.org
Today, unpaid family caregivers provide the bulk of care for older Arkansans in part because the cost of long-term care remains unaffordable for most middle income families. More than 452,000 Arkansans help their aging parents, spouses and other loved ones stay at home by providing assistance with bathing and dressing, transportation, finances, complex medical tasks like wound care and injections, and more. The value of this unpaid care totals about $4.7 billion.
“When it comes to helping older Arkansans live in the setting of their choice, family caregivers take on big responsibilities,” explains Nehus. “Many juggle full-time jobs with their caregiving duties; others provide 24/7 care for their loved ones. With every task they undertake, these family caregivers save the state money by keeping their loved ones out of costly nursing homes – most often paid for by Medicaid. They have earned some basic support.”
Arkansas ranks 26h nationally overall in Support for Family Caregivers, and 20 th in the dimensions of Supporting working caregivers and 20 th in the Nurse delegation and nurse practitioner scope of practice performance indicator. But more should be done.
That’s why AARP Arkansas fought for passage of the Arkansas Lay Caregiver Act (Act 1013 of 2015), which helps ease transitions from hospital to home for patients & their caregivers. The Caregiver Act allows patients to designate a caregiver when admitted to the hospital if the patient so desires. The designated caregiver is notified before the patient is discharged and the hospital will consult with the caregiver on how to care for the patient after he/she returns home.
AARP Arkansas also is fighting for expanding nursing scope of practice/nurse delegation. By modernizing outdated rules to broaden scope of practice, nurse practitioners will be able to do their jobs, using all their advanced training and skills to care for patients—when and where care is needed. By delegating basic health maintenance tasks to home aides, nurses will have more time and opportunity to focus on treating their patients, and support family caregivers.
The single strongest predictor of a state’s long-term care system is the reach of its Medicaid long-term care safety net. That’s why AARP is also fighting to expand services provided at home and in the community, by shifting funds away from more expensive nursing home care. While the inappropriate use of antipsychotic medication in nursing homes has decreased in Arkansas, the Scorecard highlights additional issues related to institutional care in Arkansas such as Percentage of nursing home residents with low care needs (in which Arkansas ranks 41 st nationally).
A relatively low ranking on this measure means people who do not require physical assistance in bed mobility, transferring, using the toilet, and eating, but are still in nursing homes when a less costly form of care might be more appropriate.
While Arkansas does rank 27th in the percentage of Medicaid long-term care dollars for older adults and people with physical disabilities that support care provided at home and in the community—the care setting that most Arkansas prefer—the Scorecard spotlights areas that call for improvement, especially effective transitions from one form of care to another. Specifically:
- Rank: 50—Percentage of nursing home residents with one or more potentially burdensome transitions at end of life
- Rank: 50—Percentage of new nursing home stays lasting 100 days or more (2012), with little or no change in performance
- Rank: 49—Percentage of long-stay nursing home residents hospitalized within a six-month period (2014), with little or no change in performance
“This Scorecard gives us a snapshot of how well Arkansas serves our older residents, those with disabilities, and family caregivers—and shows us where we must sharpen our focus to better assist hardworking Arkansans,” concludes Nehus. “Now is the time for policymakers to act.”

Of the 25 Scorecard indicators, many may be improved through state policy changes, pointing to the importance of AARP’s multi-state advocacy campaign, launched in 2014, to help older Americans live independently, at home, and the family caregivers that support them.
The Scorecard reveals that in less than 10 years, Boomers will begin to turn 80, placing new expectations and demands on a still imperfect long-term care system. Further, this generation will have far fewer potential family caregivers to provide unpaid help.
Long-term care (also called long-term services and supports) is a diverse set of services designed to help older people and those with disabilities; services can be provided in a person’s home, in a community setting such as an adult day center, or in a group residential facility like a nursing home.
The full state Scorecard, along with an interactive map of state rankings and information, is available at www.longtermscorecard.org.
About AARP: AARP is the nation’s largest nonprofit, nonpartisan organization dedicated to empowering Americans 50 and older to choose how they live as they age. With nearly 38 million members and offices in every state, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands, AARP works to strengthen communities and advocate for what matters most to families with a focus on health security, financial stability and personal fulfillment. AARP also works for individuals in the marketplace by sparking new solutions and allowing carefully chosen, high-quality products and services to carry the AARP name. As a trusted source for news and information, AARP produces the world’s largest circulation publications, AARP The Magazine and AARP Bulletin. To learn more, visit www.aarp.org or follow @AARP and @AARPadvocates on social media.

















)

















.jpg?crop=true&anchor=13,195&q=80&color=ffffffff&u=lywnjt&w=2008&h=1154)


























