AARP Hearing Center
By Merry MacKinnon
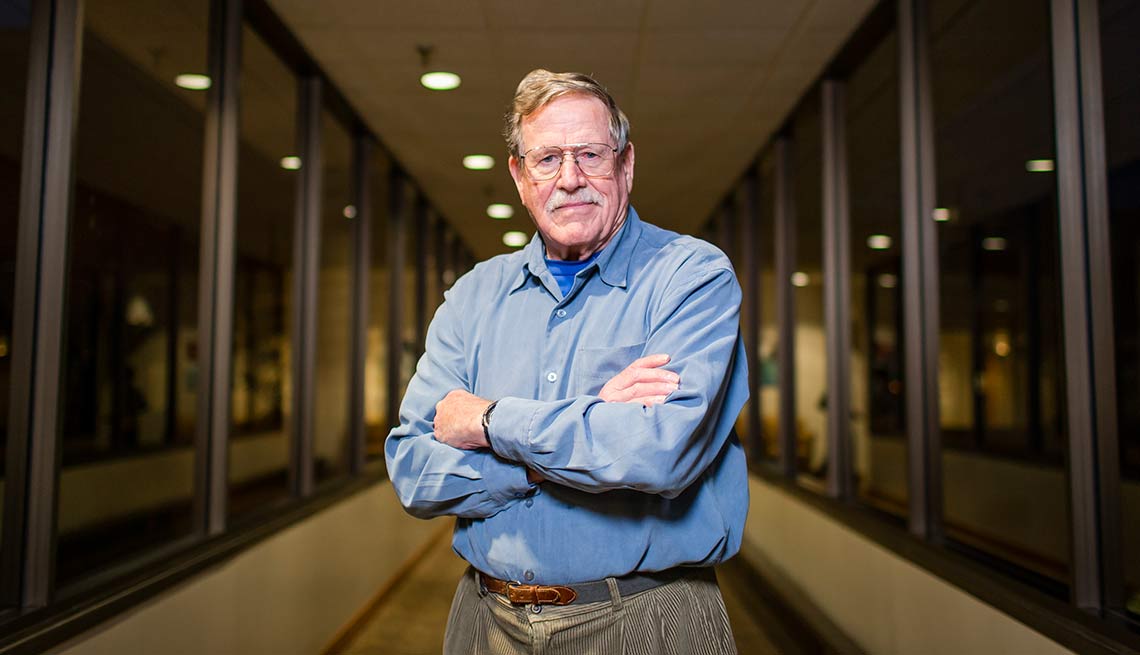
When Robert C. A. Moore heard his wife, Janie, calling to him, he hurried into the kitchen, where he found her lying on the terra-cotta floor. She had fallen and broken her hip.
Janie had her hip replaced in Mexico, where they were visiting. But after returning to Portland, she was hospitalized for replacement of the new hip.
Back home, Moore fed her, washed her, helped her onto her electric scooter and encouraged her to do her physical therapy. Both were in their late 70s.
What he didn’t know was that even personal hygiene can pose risks for a patient. No one told him how to avoid spreading bacteria when cleaning his wife. Looking back, he fears he caused Janie’s series of bladder infections. “I didn’t know how to help her,” said Moore, now 83.
As hospital stays have shortened, family caregiving has become an essential—and demanding—part of health care.
Osteoarthritis, stroke and heart failure are the most common ailments involving long-term family caregiving. Short term, accidents are the most common.
About half of the country’s 40 million family caregivers perform medical or nursing tasks: giving injections, managing medications, dressing wounds and operating medical equipment. Often these caregivers are untrained. And sometimes they make mistakes.
“Medical professionals sometimes assume that people know how to do these things,” Moore said. “But, for the caregiver, it can be trial and error.”
Working together
Moore, an AARP volunteer, testified last spring before the state Senate Health Care Committee in support of the Caregiver Advise, Record, Enable (CARE) Act. It passed unanimously.
“What’s exciting about the CARE Act is it sets into statute that hospitals reach out to caregivers and say, ‘We want you to be involved,’ ” said Jerry Cohen, AARP Oregon state director.
Effective Jan. 1, hospitals must record, on admission, the patient’s designated family caregiver if the patient identifies one. Examples are unpaid relatives, friends or significant others.
Upon the patient’s discharge, the hospital must offer to share discharge planning with the caregiver and provide guidance on medical and nursing tasks that are relevant to the patient’s condition and based on the caregiver’s ability.
Whether the tasks involve changing gauze or giving shots, instructions are supposed to be case-specific, depending on what the caregiver and hospital identify as needed.
Instruction might include live demonstrations provided by hospital staff or videos for the caregiver to review.
“The point is to go beyond basic instruction-sheet handouts,” Cohen said.
So far, 18 states have passed a version of the CARE Act, and many more are considering it. In Oregon, the hospital association supported the legislation.
The Oregon Association of Hospitals and Health Systems worked with AARP Oregon to develop the legislation, which “extends the continuity of care and aligns with current hospital discharge practices,” said Philip Schmidt, OAHHS associate vice president for public affairs.
For example, Kaiser Permanente’s existing programs to reduce rehospitalization rates fit well with the CARE Act, said Rahul Rastogi, M.D., chief operations officer for Northwest Permanente.
“We’re pleased to be part of this important statewide effort to ensure caregivers have the resources and support they need,” he said.
Though Moore’s own caregiving ended in 2013 with Janie’s death at 81, he is delighted that the CARE Act is now law.
“A caregiver wants to do the right thing, but doesn’t always know what it is,” Moore said.
Merry MacKinnon is a writer living in Portland, Ore.































































