AARP Hearing Center
Virginia ranks 19 th when it comes to meeting the long-term care needs of older residents, but AARP warns more must be done, at an accelerated pace, to improve quality of life and quality of care, support for family caregivers, and effective transitions. This is according to a new, comprehensive state-by-state Scorecard from AARP with support from the nation’s leading organizations behind quality long-term care, The Commonwealth Fund and SCAN Foundation.
Raising Expectations 2014: A State Scorecard on Long-Term Services and Supports for Older Adults, People with Physical Disabilities, and Family Caregivers – an update of the inaugural 2011 Scorecard – ranks each state overall and within 26 performance indicators along five key dimensions: affordability and access; choice of setting and provider; quality of life and quality of care; support for family caregivers; and effective transitions. New indicators this year include length of stay in nursing homes and use of anti-psychotic drugs by nursing homes, raising serious concerns about the quality of institutional care.
“The vast majority of older Virginians want to live independently, at home, as they age – most with the help of unpaid family caregivers,” says Bill Kallio, state director of AARP Virginia, which serves more than 1 million members age 50 and older in Virginia. “Even facing tight budgets following the Great Recession, Virginia is making some progress to help our older residents achieve that goal. However, this Scorecard shows we have more to do – and we don’t have time to stand idle.”
Today, unpaid family caregivers provide the bulk of care for older Virginians, in part because the cost of long-term care remains unaffordable for most middle income families. In Virginia, more than 1.7 million residents help their aging parents, spouses, and other loved ones stay at home by providing assistance with bathing and dressing, transportation, finances, complex medical tasks like wound care and injections, and more. The value of this unpaid care totals about $11.7 billion.
“When it comes to helping older Virginians live in the setting of their choice, this silent army of family caregivers assumes the lion’s share of responsibility,” explains Kallio. “Many juggle full-time jobs with their caregiving duties; others provide 24/7 care for their loved ones. With every task they undertake, these family caregivers save the state money by keeping their loved ones out of costly nursing homes – most often paid for by Medicaid. They have earned some basic support.”
According to the state Scorecard, many family caregivers (60.4 percent) face a degree of stress and worry. That’s why AARP Virginia is fighting for the Caregiver, Advise, Record, Enable (CARE) Act and funding for respite care.
The CARE Act will help family caregivers when their loved ones go into the hospital – and as they return home. Specifically, the CARE Act will require hospitals to:
- Record the name of the family caregiver when his/her loved one is admitted.
- Notify the family caregiver when his/her loved one is to be moved or discharged.
- Give instructions for the tasks the family caregiver will need to perform while caring for his/her loved one at home.
Respite care helps to support family caregivers who are on call 24 hours a day, seven days a week, by giving them a hard-earned, well-deserved break – allowing them to recharge and continue the essential roles they serve in safely caring for their loved ones. Family caregivers often put aside their own needs – skipping doctors’ appointments, developing poor eating habits, and not getting enough sleep.
The single strongest predictor of a state’s long-term care system is the reach of its Medicaid long-term care safety net. That’s why AARP is also fighting to expand services provided at home and in the community, by shifting funds away from low-quality, more expensive nursing home care. The Scorecard highlights concerns about institutional care in Virginia: residents with pressure sores, staff turnover, and use of antipsychotic medication.
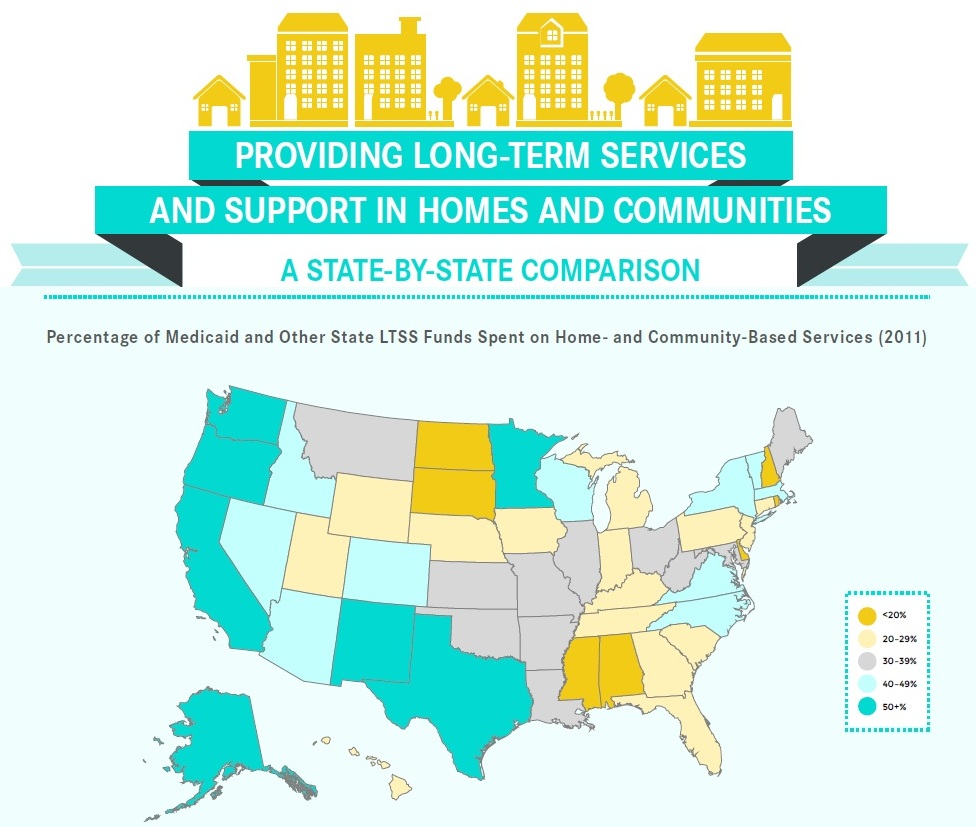
While Virginia does rank 17 th in increasing the percentage of Medicaid long-term care dollars that support care provided at home and in the community – the care setting that most Virginians prefer – the Scorecard spotlights areas that call for improvement, including choice of setting and provider, quality of life and quality of care, and effective transitions. Specifically:
- 41 percent of Medicaid and state-funded long-term services and supports go towards home- and community-based services for older adults and adults with physical disabilities.
- 13.7 per 1,000 adults receive participant-directed services through Medicaid.
- 73.5 percent of adults with disabilities in the community receive needed support.
- 87.4 percent of adults with disabilities in the community were satisfied.
- 8.5 percent of adults with 90+ day nursing home stays successfully transitioned back to the community.
“This Scorecard gives us a snapshot of how well Virginia serves our older residents, those with disabilities, and family caregivers – and shows us where we must sharpen our focus to better assist hardworking Virginians,” concludes Kallio. “Now is the time for policymakers to act.”
Of the 26 Scorecard indicators, 13 may be improved through state policy changes, pointing to the importance of AARP’s multi-state advocacy campaign, launched this year, to help older Americans live independently at home, and the family caregivers that support them. Currently, 42 states are advocating as part of the campaign, including Virginia.
The Scorecard reveals, in just 12 years, the leading edge of the Baby Boom Generation will enter their 80s, placing new demands on a still imperfect long-term care system. Further, this generation will have far fewer potential family caregivers to provide unpaid help.
Long-term care (also called long-term services and supports) is a diverse set of services designed to help older people and those with disabilities; services can be provided in a person’s home, in a community setting such as an adult day center, or in a group residential facility like a nursing home.
The full state Scorecard, along with an interactive map of state rankings and information, is available at www.longtermscorecard.org.































































