AARP Eye Center

In January 2023, Jean and Bob Brown, both in their 80s, moved from Florida to Kennesaw, Georgia, to live with their son Randy.
The decision to leave a state that had been home for 20 years came after Randy and his siblings grew concerned about their parents’ ability to continue living alone. They were worried about Jean’s ability to care for her husband, who has dementia, as well as her own health problems.
“The alternative was a nursing home because I didn’t know how much longer I could handle him,” Jean says. In the previous six months, she had twice fallen and injured herself. And while the transition has been a bit rough, the Browns were helped by Empowerline, a service that receives government funding in part to help Georgians navigate such situations. “I was ready for the challenge ... but I was just still kind of lost,” says Randy, 58. “I didn’t know what was involved in caregiving.”

Services such as Empowerline — part of Georgia’s Aging and Disability Resource Connection network — are part of a nationwide effort to help people age in their homes, rather than institutional settings. That’s according to new data from AARP’s latest Long-Term Services and Supports State Scorecard, which uses 50 spending, quality and access indicators to rank each state’s long-term care system.
Shift part of nationwide effort
The availability of services like Empowerline contributed to Georgia’s number 15 ranking among states in the category that tracks aging and disability resources. Launched in 2018, Empowerline provides connections to privately and publicly funded resources from more than 26,000 community-based providers.
Georgia wasn’t alone: 33 states and the District of Columbia improved in the same category; just 11 saw a decline, and six held steady.
EXPLORE: AARP Long-Term Care Scorecard
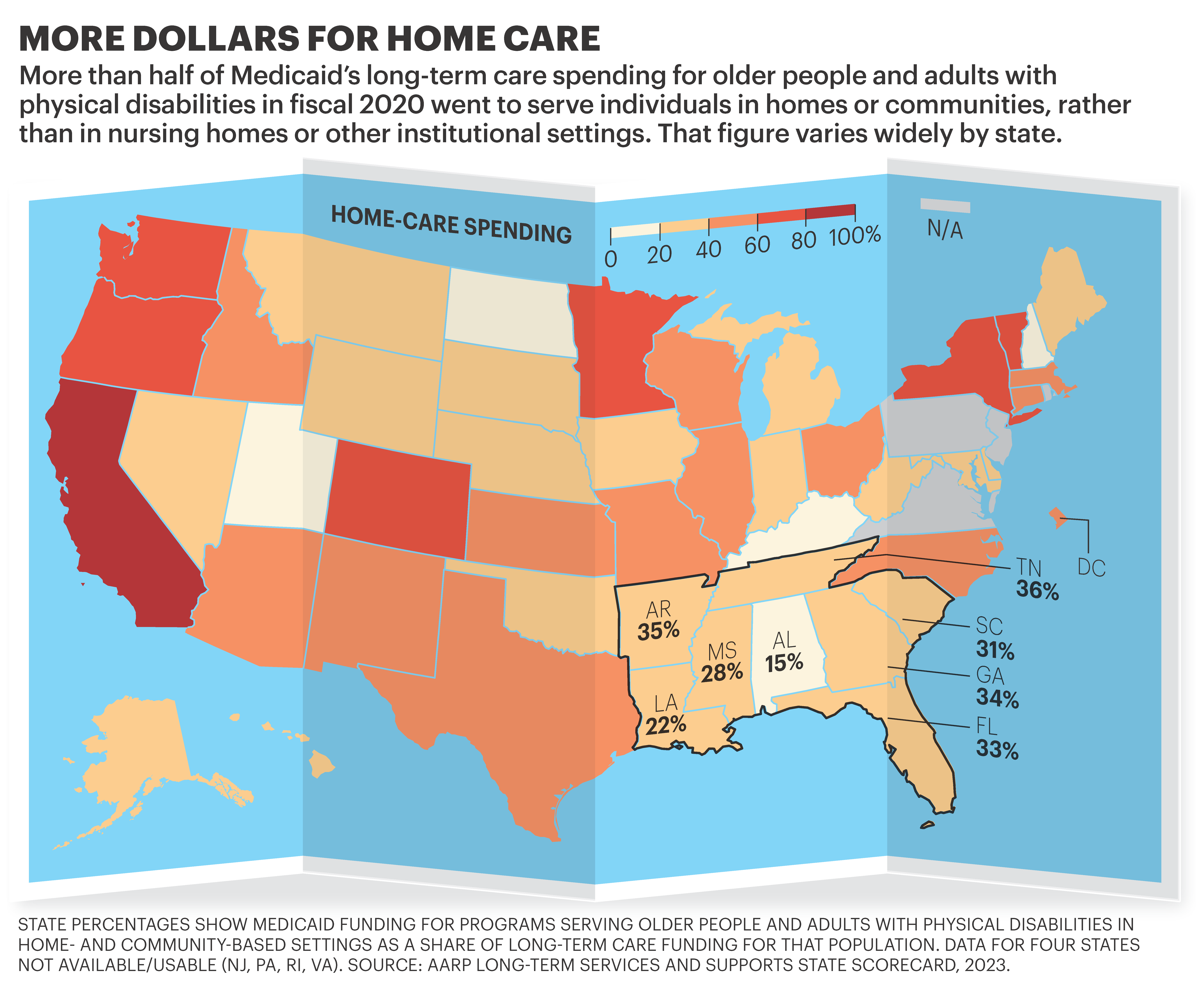
Beyond that, the Scorecard shows that for the first time since AARP began publishing it in 2011, more than half of Medicaid’s long-term care dollars nationwide for older people and adults with physical disabilities went to home- and community-based services instead of nursing homes or other facilities.
“This is a big deal. We are seeing a breaking point,” says Susan Reinhard, senior vice president of AARP’s Public Policy Institute, which published the Scorecard in September.
The shift to home- and community-based services comes as demand for such care has increased, fueled in part by a pandemic that took a horrific toll on nursing home residents. Polls have consistently shown that most older Americans want to age in place.
But with America’s population of older adults growing, the chasm between the availability of HCBS and access to such services is poised to widen. “We’re going see a dramatic increase in the 80-plus and 85-plus population” as the boomer generation gets older, says Robert Applebaum, a senior research scholar at Miami University’s Scripps Gerontology Center in Ohio. “So the demand for long term services ... is going to be tremendous.”
In Georgia, the Browns show one way for states to address that demand.
After Randy found Empowerline, caregiver specialist lead Alyssa Perkins connected him to organizations that provide support and advice on how to help his parents — including how to deal with his mom as she struggled with a loss of autonomy. Perkins helps callers get advice on transportation options, home repair and other available services.
Randy says he and Jean learned how to communicate more effectively with Bob so that he still feels empowered.
“I definitely learned some things, and we kind of settled into this more comfortable way of dealing with the environment,” Randy says. He is helping his parents apply to Georgia’s Elderly and Disabled Waiver Program, which provides HCBS to recipients of Medicaid, the federal-state program for low-income Americans that often pays for long-term care. Medicaid programs aren’t required to cover HCBS, although states may do so through a waiver program or by including optional services in their state plan.
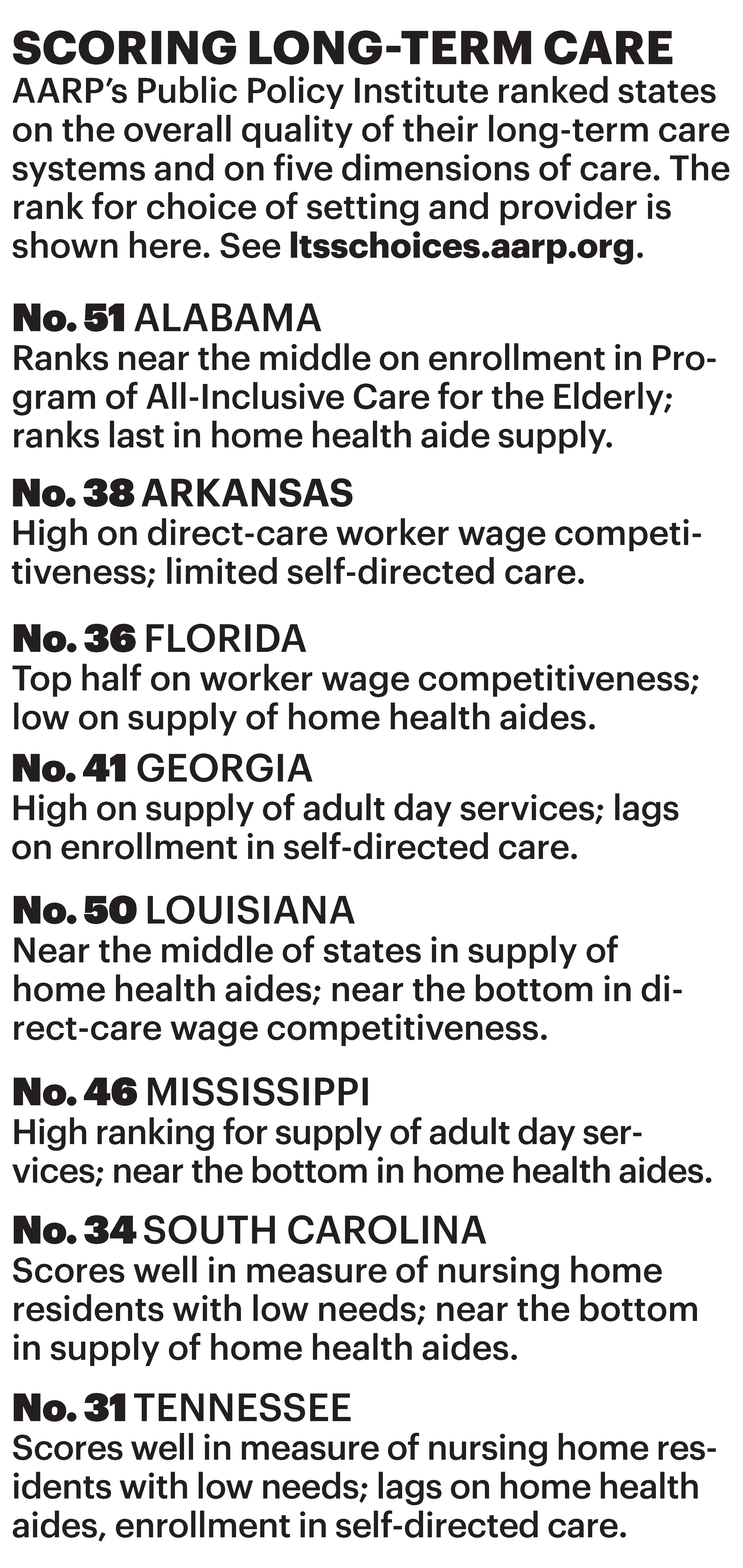
Despite its improvement in several Scorecard categories, Georgia’s long-term care system overall ranked just 39th in the nation.
In the Southeast, Florida, Georgia and Tennessee boosted their share of dollars going toward HCBS — although all states in the region ranked in the bottom half of the country on that measure.
Waiver cuts wait times
Since the 1980s, Georgia has had a Medicaid-funded waiver for HCBS, meaning eligible people generally don’t have to endure long waits for services, says Becky Kurtz, senior managing director of the Atlanta Regional Commission’s Aging & Independence Services. “It takes a little bit of time to go through all the administrative pieces to get the services actually in your home started — but it’s not like you’re waiting for months or years like used to be the case,” she says.
However, residents who don’t qualify for Medicaid-funded HCBS face “very long waiting lists” for services like home care and meal delivery, Kurtz says. In metro Atlanta alone, more than 4,000 eligible people are on a waiting list for home-delivered meals, she says. In fiscal 2022, the commission provided meals, personal care and homemaking to more than 15,000 people and also distributed about $580,000 in respite vouchers for caregivers, says its annual report; it also recorded more than 67,000 visits to Empowerline’s website, up 11 percent from the previous year.
The Tennessee Coalition for Better Aging is pushing state leaders to reimagine its long-term services and supports system, says cochair Grace Sutherland Smith, who is also executive director of the nonprofit AgeWell Middle Tennessee.
During recent years, the state has allocated more funding for the Medicaid waiver TennCare CHOICES program and the state-run Options for Community Living, which advocates see as a win. “We’re catching folks earlier ... so we’re able to provide a limited package of service to them earlier — before they reach that nursing home level of care that’s required to get into CHOICES,” says Aaron Bradley, a longtime advocate and the director of the East Tennessee Area Agency on Aging and Disability.
But a direct-care worker shortage is impacting the delivery of HCBS in states across the nation. “We have money to spend,” Bradley says. “We have people waiting on service — several thousand actually statewide waiting on service — and home care providers cannot hire staff.”
Julie Rasicot, a writer and editor and former online news managing editor in Montgomery County, Maryland, writes regularly for the AARP Bulletin.
More on Home Care
- Care Companions: A Watchful Eye and Willing Ear for Older Adults
- Find the Right Home Aide for Your Loved One
- AARP Survey: 8 in 10 Older Adults Want to Age at Home